Perverse Incentives in Healthcare
COVID diagnosis, Hospital Admissions, Vaccines, Remdesevir, Intubation, and more
Even an animal can understand a carrot and stick, but too often it seems those in charge haven't the slightest idea what the knock on effects of their perverse incentives will be.
Excusing stupidity, instead of assuming malice is the usual tack, that is probably wrong and even if it isn’t we should just demand better and punish either one.
The incentives are developed like this: industry generally spends millions on high priced lawyers to “help” legislators craft the rules that supposedly govern industry participants.
In practice regulations only benefit the largest incumbents and crowd out competitors, while enriching those who wrote and passed the laws.
A good rule of thumb is that any time an industry is begging for regulation it is in order to raise prices, stifle innovation and accrue treasure to itself.
We have seen the latest iteration of this in the Artificial Intelligence space, with Elon Musk insisting that AI super-intelligence is the greatest threat we have ever faced (talk about hyperbole, this is climate alarmism squared), and OpenAI founder Sam Altman (of ChatGPT fame) heading to Capitol Hill to welcome government regulation with open arms. These industry executives simply want to create barriers to the two kids-in-a-garage companies that historically disrupted entire industries, but can’t pay for a dozen high priced lawyers to comply with 1200 pages of fine print regulations.
In medicine we’ve had perverse incentives for ages.
I worked for 1 decade in hospitals and saw first hand how this worked.
Insurance companies like Medicare pay per admission rather than by day, depending on the diagnoses.
So for example someone is admitted with pneumonia and a heart attack and later develops hyponatremia.
The hospital sends these 3 diagnoses to the insurance company and gets paid, say $100k.
Now here’s the rub: the hospital gets the same amount whether they kept the patient for 3 days or 300 days.
So obviously it’s in the hospitals best financial interest to discharge patients as soon as humanly possible, which is why every hospital I worked in had a discharge planner who would go around and keep an eye on each patient and nudge doctors constantly once they (the discharge planner) thought a patient was likely OK to discharge.
Ultimately the doctor has the final say and I never came across a heavy handed discharge planner that was very pushy, but the very fact they are around creates a subconscious and conscious pressure to discharge patients sooner rather than later, though I will also admit that in some cases they are right to give some pushback to a doctor, since we aren’t always considering whether the patient actually needs to remain under our care another day or not, so much as just taking care of them as long as they are present - that care will continue after discharge, whether at home, or in a nursing home, or some other intermediate facility.
On the other hand it’s also in a hospitals best interest to admit as many patients as possible rather than send them home from the ER, since each admission carries a guaranteed payment (as long as it meets the basic requirements for admission).
So in practice if there are any beds available administration will urge the ER doctor to admit more patients.
If the hospital is full administration will beg/cajole the hospital doctors to discharge as quickly as possible from the inpatient wards so the ER can start admitting more.
As one incentive leads to gaming the system, other incentives or disincentives are later added to try to counteract the negative effect of the first incentive, they then create further negative effects requiring even more carrots and sticks to be added to try to achieve the end goal of patient care.
All of this complexity adds layers of middle management and cost.
For example going back to the admission issue, since hospitals were incentivized to admit as many as possible, insurance companies then had to push back and create admission criteria. Hospitals could no longer just admit grandma because she was lonely on Christmas Eve - yes things like this used to happen and still do - since there is almost always a way to game any incentive structure:
With the lonely grandma who calls up EMS because she feels “sick” on Christmas Eve the excitement of being wheeled into the ER might spike her blood pressure and heart rate for a few minutes, a urinalysis and urine culture can be counted on to come back looking a bit off in most elderly women, maybe the pulse ox that measures oxygenation slipped for a few minutes and registered a “low” blood oxygen reading, maybe there’s a weird squiggle on her EKG, or a slightly suspicious shadowy area of her CXR due to a fold in her shirt being misread as a possible pneumonia, I think you get the picture
There is enough uncertainty built into diagnosis in medicine that physicians can very easily argue for an admission for some completely unrelated social reason.
What’s a lot more common than lonely grandmas is “unsafe” discharges. Someone elderly or frail doesn’t have someone to receive them at home, soothed have to stay in the hospital, unfortunately the longer they stay in the hospital the more frail they become because we don’t let them out of bed for fear they’ll fall, but I digress.
COVID PANDEMIC INCENTIVES
Much has been exposed about the perverse pandemic incentive structures. We know that hospitals were paid 10s of thousands of dollars for each admission that had a diagnosis of COVID-19, they were paid extra if Remdesevir was administered, if a patient was intubated, etc. In some places there may have been incentives for following specific protocols that included sedatives, or disincentives for not following them.
People see these incentives and wonder if some nefarious group of people designed them specifically to pad the pandemic numbers and kill people with ventilators and Remdesevir.
At this point I suspect that at the top of the medical hierarchy it was known to some people that Remdesevir was a deadly drug, though promisingly expensive drug, that was like a round peg that had failed to fit into prior square shaped holes and COVID was yet another squarish hole it didn’t belong in.
The reason hospitals were given extra payments for COVID cases, Remdesevir, and intubations was because those were considered markers of increased severity of illness. They form part of the usual calculus that decides how much any hospital admission will be paid.
Going back to earlier, the hospital counts up the diagnoses that were made, and whether certain things had to be done, and each of those things has a dollar amount that contributes towards the total payment for that admission.
So although most people probably think these incentive payments were unusual, but they were just business as usual.
They are not seen as “incentives”, rather as markers of severity that might for example predict how much capital and resources the hospital has to use to care for that patient. Resources including specialists, tests, days spent in the hospital, etc.
From an economic perspective it appears that hospitals are incentivized to convince insurers that their patients are as sick as possible, and that is true.
There is an entire department that combs through the medical records created by doctors, nurses and other support staff to collect all the diagnoses and tests and evidence of severity of illness and submit it to the insurance company so that the hospital gets its due.
This does not mean as a routine matter of fact that the doctor at the bedside is thinking to himself, “if I prescribe Remdesevir I’ll make a few extra bucks” (though if that were the case he would also have been programmed to think that it’s a win win).
But it does mean that someone in administration tasked with maximizing revenues knows that Remdesevir is a big money maker, so they look at prescribing practices and of they see that it looks like their doctors aren’t making much use of Remdesevir, they may decide to spearhead an educational initiative for their doctors, probably sponsored by the manufacturer, or they may just recommend to all their hospital doctors to get an infectious disease specialist consult on each COVID case, because they can count on the infectious disease specialists to be clued in to the latest guidelines recommending Remdesevir.
Ultimately the society guidelines are what 99% of physicians follow religiously. If they are told you are veering outside practice guidelines, it means that you’re veering outside the safe scope of practice. If a bad outcome were to occur and the case went to malpractice practicing within the guidelines essentially guarantees a physicians economic and professional safety.
Protect Yourself from Threats to Your Health
Get COVID protocols (ivermectin!), prepper antibiotics, and more.
Physicians have generally learned to distrust their own lived experience in favor of what the guidelines recommend.
This makes sense in much of medicine where the efficacy levels of so many drugs are miniscule. A single physicians experience could easily be wrong when there’s say a 2% chance of benefit from a drug.
In many cases the drugs being prescribed have no immediate observable benefits, aside from classes of drugs used for acute problems like infections, or chronic conditions that can acutely worsen like diabetes or hypertension.
Statins are a good example of a common chronic disease medication that doesn’t provide much feedback to physicians outside of changes in lab values. Patients either have another stroke or heart attack in the coming years or they don’t. The supposed benefit of a statin is that out of 100 people who had a previous heart attack, 2 will have another heart attack if none of the 100 take a statin, but if all 100 take a statin then only 1 of them will have another heart attack.
On the other hand 2 of the hundred taking statins will also likely develop diabetes … which itself is a risk factor for heart attacks and strokes, so go figure.
The point being there are many factors that can interfere and give someone a stroke or heart attack. Statin use is a small absolute factor in that mix, and in the lived experience of physicians when statins started being prescribed there was no noticeable decrease in rates of heart attacks or strokes in their patient populations.
Even if there had been a 1% drop, it would be hard to notice such a small change.
In the example of Remdesevir given to someone for worsening COVID-19, who then develops kidney failure and dies, most doctors will assume that it would have been the same if they hadn’t received Remdesevir, and that some percent of those who make it with Remdesevir, made it because of the Remdesevir, and they will assume this even if in their own experience patients start dying more frequently once Remdesevir starts being used, because they will figure that the rise in deaths is due to some other random change, like sicker patients happening to show up that week, or even a shift in the lethality of the viral strain.
OUTPATIENT MEDICINE
My experience was in hospitals, but outpatient medicine is another story (I also worked as an independent contractor, so employed physicians in hospitals may have had more direct incentive programs for prescribing certain medications).
I do know that in outpatient medicine, doctors are directly incentivized to prescribe certain medications.
Why are certain medications chosen for incentives?
Statins have been incentivized for a long time and they are a multibillion dollar market.
Industry wants to sell more statins, they are incentivized to expand the indications as much as possible, to bring as many patients under the statin indication umbrella as they can - which famously produces such ridiculous recommendations from the biggest industry boosters as putting statins in the water supply.
But the biggest and most widespread incentive structure in modern medicine (pre COVID-19) probably exists for pediatricians and the childhood vaccination schedule (close runners-up are likely chemotherapy and dialysis).
40+ Hours of Free Video Content on Spike Protein Diseases
In fact you could consider most of the pediatrics profession to simply be a vaccine administration arm of the DOD.
You see vaccine technology is considered a matter of national defense. As such we need to maintain our manufacturing capacity and research pipelines and continue pumping out vaccines, because one day we, or our troops may face a bio terror threat requiring a thriving vaccine industry to neutralize.
So this massive structure needs to be kept running year in year out across the decades and generations, and the best way to do that is to put as many shots in arms as possible.
A significant amount of money pediatricians make come from vaccine incentive programs and the fee for administering vaccines.
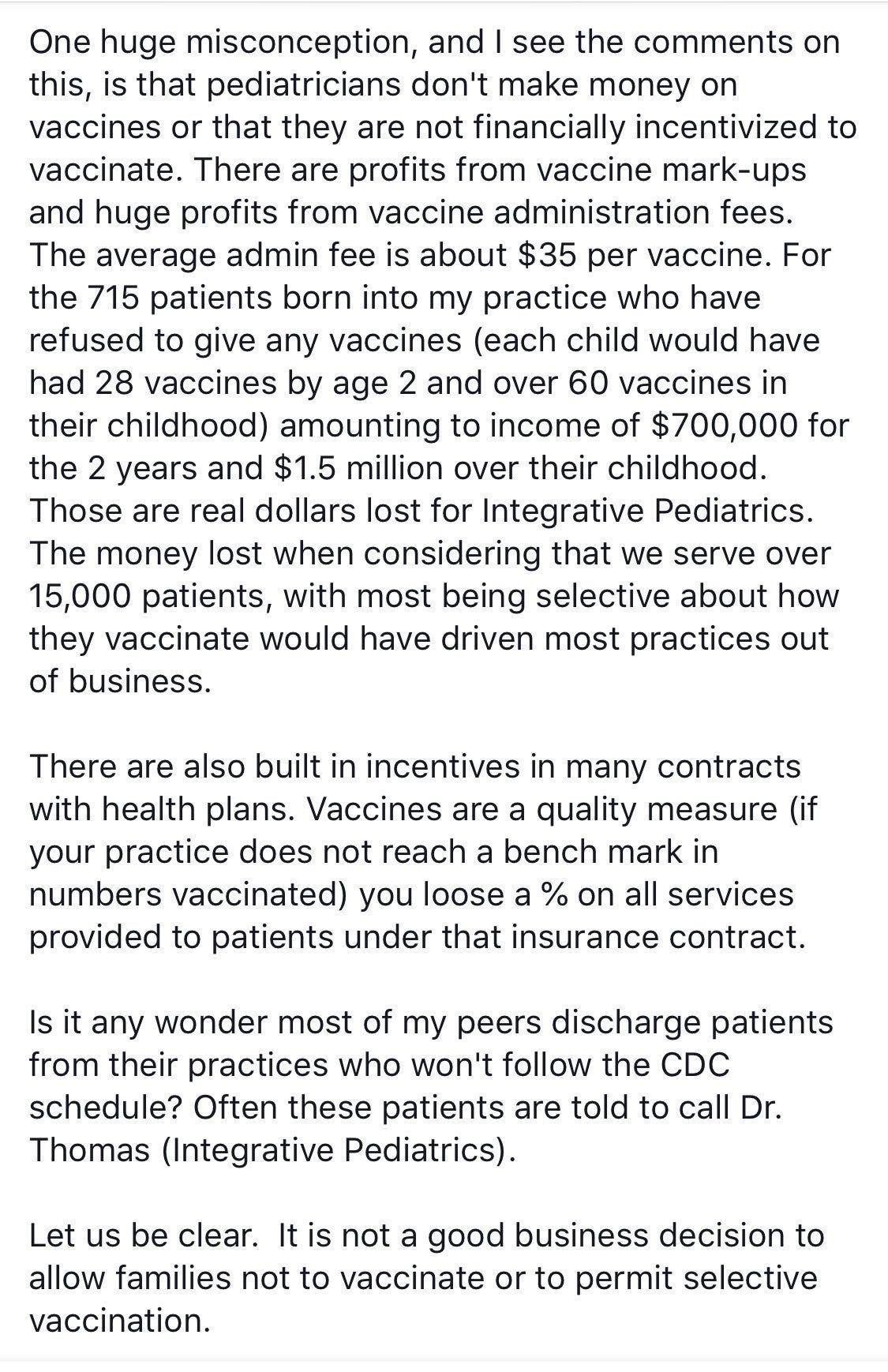
Paul Thomas, MD famously runs an integrative pediatrics practice that published a peer reviewed study comparing results for vaxxed and unvaxxed children in his very large 16,000 strong practice.

The results created a tremendous furor at the medical board and his license was revoked. The paper was also forcefully retracted, but is still available to read.
Here Dr Thomas explains in his own words the incentives around vaccines, and the amount of money his practice loses for not vaccinating:
So let’s run some more numbers here, because 1 vaccine administration fee of $35 doesn’t sound like much, but we’ll see.
An average pediatrics practice has 1500 patients per provider (some have twice as much or more).
Those 1500 patients get 60 shots over the course of birth to 18 years, which is 1,620,000 shots administered in 18 years, or an average of 5,000 vaccines administered per year. That’s $175,000 in vaccine administration fees alone at $35 a pop.
This is essentially the median salary of a pediatrician. Of course most practices bring in about double to account for their overhead expenses, which run 50-60%. But without the $35 payments there would be basically nothing left over. Pediatrics is not economic for the most part without vaccines.
So it is not hyperbole when Dr Thomas says most practices would be driven out of business if they do not vaccinate.
Which means most pediatricians really only exist to administer vaccines in “wellness” visits because I would argue that they are then conveniently around to deal with all of the illnesses that stem from having given the vaccines in future “sick” visits (in other words vax injury visits).
And of course pediatrics is then the feeder to the adult medicine industry.
Now here’s an example of COVID-19 vaccine incentives, which are even more lucrative than anything I’ve ever seen in pediatrics (there may be childhood vaccine incentive structures like this out there, I’ve just never seen them myself).
So let’s run some number with the above. Again lets take a mid size practice of 1500 patients, and just assume that they all have the above incentives (in practice there are many different insurance plans and some will provide better or worse incentives or even none at all).
So in our imaginary practice let’s say 30% of 1500 patients (450) get the initial COVID-19 shot and 30% (450) also get the second shot by Dec 1, 2021. In that case the practice would make $20 x 450 = $9000 for the first shot and $100 x 450 = $45,000 for the second shot, for a total of $54,000 in additional revenue for 2021.
Now lets see the maximum this practice could have made if all members were vaccinated, in which case bonus payments rise as described in the letter above:
For the first shot: 1500 patients x $125 = $187,500, and for the second shot: 1500 x $250 = $375,000, for a combined total of $562,500 in additional income for a relatively small practice of only 1500 patients.
The average income of a primary care doctor in the US is about $200,000, on revenue of probably $400,000-500,000. This single incentive plan could have doubled practice revenue in 2021.
What’s even more shocking about the numbers for me is that this was a Medicaid managed care plan. Medicaid is usually the stingiest of insurance plans, and the highest compensated practices in the country usually have the lowest percentage of Medicaid patients. I can only imagine how much providers were paid by Medicare or the more expensive private employer insurance plans.
PARADIGMS
People live within a false paradigm that their doctors visits improve their health or prevent illness, when in fact the more contact someone has with doctors the more sick they are likely to be and the more sick they are likely to become.
And this isn’t just a matter of diagnosing something that was already there, it literally means creating illness that did not previously exist and I’m sure that perverse incentives have a lot to do with this.
Good examples can be had from the pandemic, where early on during lockdowns cardiologists noted an unusual drop in heart attack deaths when patients started seeing their doctors less often and showing up to the hospital less often.
Presumably they remained on their usual medications, though most patients have very poor rates of adherence, which likely dropped further when not following up in person for routine visits, even if refills were being sent in.
The biggest difference then was probably in routine care for heart attacks administered in hospitals.
It is possible that on average our care of heart attacks kills more people than it saves, but good luck convincing anyone to do anything different during an actual heart attack, whether patient or physician, because who knows what element of the care is useful and what is harmful?
Is it too many fluids, too many blood draws? Too much blue light, too many EMFs, not enough sleep? Is it actual forced adherence to meds that were poorly adhered to at home? Is it just the cumulative stress of being hospitalized?
Lifestyle optimization is the way to go, and taper off any medications if at all possible. Small and simple tweaks can resolve most issues, and then for anything left over a good alternative health practitioner can often fix up the rest.
Group coaching is the single most effective way to change lifestyle habits for good and put one small baby step in front of the other, which is why I created the Lean Vitality program with Health Coach Bethany Stewart.
We take new cohorts every 2 months, but you can also get started reviewing course materials right away.
There is somewhat of a focus on weight loss, since most people struggle with that, but the program is really for anyone who wants to optimize their lifestyle (which automatically includes getting leaner and stronger).
Of course if you’re dealing with spike toxicity like Long COVID or Vax injury then our dedicated course, the Phoenix Protocol would be a better place to start.













Facts like this are the very reason why many people that I speak with tell me they are afraid to go to the hospital. The more we find out the more the people lose their trust in the medical profession. if indeed they have any trust or faith in the system now. It's sad that money takes precedence over one's health.
Thank you so much Dr. Haider for all you do! You prescribed Ivermectin for my husband and myself early on because we were fortunate to know the sad truth about Covid. We knew enough not to be vaccinated and were heartbroken when most of the people we knew bought into the tragic propaganda.
Every day I hope more and more people will open their eyes. We are all responsible for helping them do that! You are one of the great heroes Dr. Haider!