Some of the most common Long COVID & Vax injury symptoms include brain fog, fatigue, depression, anxiety, tinnitus, loss of taste/smell, and insomnia.
All of these can be due to inflammation in the brain.
Unfortunately most doctors cannot diagnose the brain inflammation due to spike protein.
In many cases patients can get better and fully recover with a trial and error approach: e.g. trying the various recommended anti-inflammatory meds and supplements on my Long COVID/Vax Injury Protocol.
For example I’ve now seen countless patients who had one or more of the above symptoms fully recover after just taking ivermectin - even though it doesn’t cross the blood brain barrier.
That’s probably because the primary issue wasn’t in the brain even though it was being manifested with neurological symptoms.
For example the brain tissue is completely permeated by blood vessels, but they are not considered to be inside the brain tissue itself.
Kind of like the way what’s in your stomach is technically outside your body: things you eat have to be absorbed into your body.
Similarly the blood vessels penetrate the brain in the way the gastrointestinal track (GIT) penetrates our body, but the same way the GIT chooses what to absorb, the blood vessels in the brain usually only let some things pass through, while blocking others.
Inflammatory markers originating from the body or blood vessels can leak into the brain causing problems. Dealing with the source of the inflammation will stop the release of inflammatory mediators and the neurological symptoms with them.
But in some cases the problem is in the brain itself. The spike protein for example can pass through the blood brain barrier as can the lipid nanoparticles in the shots.
Oral steroids and fluvoxamine both pass into the brain and often work great for inflammation, but some patients still struggle to improve, or hit a wall where improvement stops or they aren’t willing to proceed with other therapeutic options.
In these cases it would be helpful to have more specific tests available that would help track improvement that is happening slowly, and which could point to specific therapies.
There are a small handful of standard blood tests for inflammation: CBC with differential (looking for elevated immune system white cells), ESR and CRP.
These can be helpful for systemic acute (new onset) inflammation, but chronic brain inflammation doesn’t lead to elevations of these markers, so most physicians are blind to it's existence.
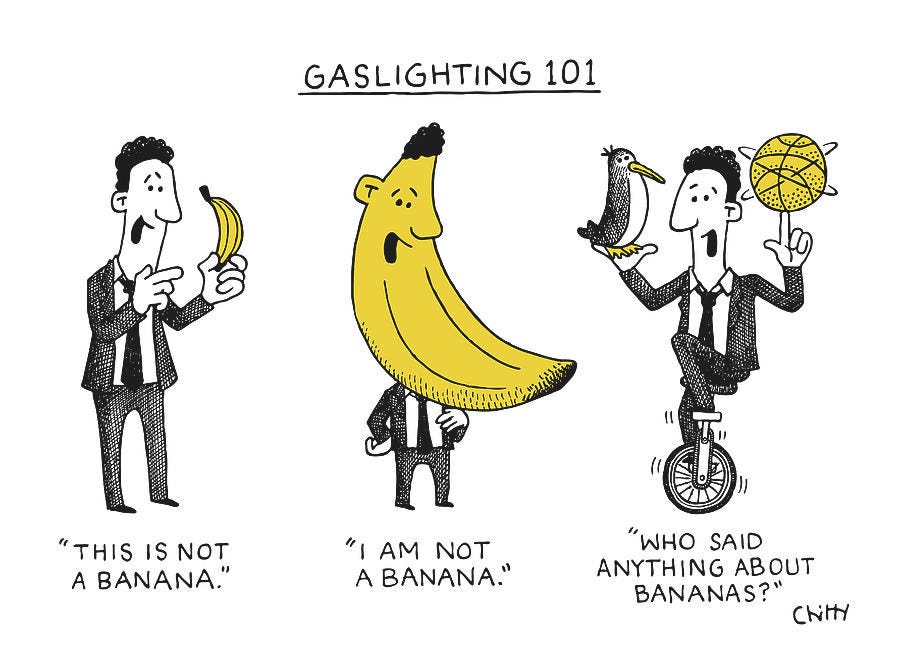
If they can’t test for it, it doesn’t exist and they refer you to psychiatry.
This is the familiar experience of most long haulers: sorry I can’t find anything wrong with you, maybe it’s just stress.
If you’re lucky they will acknowledge it could be due to the virus, but they just have no approved treatment.
If you’re lottery-winner-level lucky they will acknowledge it could be due to the shot, but again they will throw up their hands.
If you’re unlucky they’ll gaslight you or put you on a random antidepressant that has no specific effect on the underlying neuro-inflammation.
But there are actually some very specific tests that can be done which will reveal whether or not you have chronic inflammation in and around the brain.
The areas we are looking at include the blood brain barrier, which is made up of the cells lining the blood vessels of the brain, as well as brain tissue itself.
First we can test directly for damage to neurons with NSE (neuron specific enolase).
Second, there is almost always significant vascular inflammation in long COVID & Vax injury, which can be revealed by tests like VEGF and sCD40L, but we can also test specifically for breakdown of the blood brain barrier with S-100, alpha-1-antitrypsin, and zonulin.
Third, we can test for inflammation within the brain itself by looking at the activity of the enzymes IDO (indoleamine 2, 3-dioxygenase) and KMO (kynurenine monooxygenase). In the presence of inflammation these enzymes break down the amino acid tryptophan to the inflammatory molecules quinoline and kynurenine, which can also be tested for (and are probably more readily available in an organic acids in the urine test).
This inflammatory breakdown pathway can throw off a lot of brain and body functions, because tryptophan is supposed to be converted into serotonin and melatonin, two substances that are crucially important for brain and overall health.
Serotonin is important for mood, sleep, digestion, nausea, wound healing, bone health, blood clotting and sexual desire.
Melatonin is the primary sleep hormone in control of our circadian rhythm. It’s produced in the pineal gland of the brain and only in the absence of blue light (why it’s important to wear blue blockers at night)
Melatonin also stimulates tissue regeneration and is the bodies most powerful antioxidant, while helping stimulate production and recycling of other important antioxidants like glutathione.
Melatonin also increases the number and efficiency of mitochondria, the energy powerhouses of cells and helps protect them from damage.
Another important amino acid that can be sent down the wrong pathway by inflammation is tyrosine, which is usually used to make the neurotransmitter dopamine as well as thyroid hormone.
In the presence of brain inflammation the nitrogen radical peroxynitrite converts the amino acid tyrosine to nitro tyrosine making it unusable for dopamine or thyroid hormone production.
Dopamine deficiency can lead to trouble concentrating, decreased performance, fatigue unrelieved by sleep, depression and pessimism, and a lack of motivation.
Low thyroid hormone can have similar effects to dopamine deficiency as well as weight gain, muscle aches, stiffness and weakness, cold sensitivity, constipation, coarse thinning hair and dry skin, irregular menstruation, puffy face, hoarse voice and slow heart rate.
Many of these symptoms will be familiar to those who’ve suffered from Long COVID and Vax injuries.
TREATMENT
To mop up free radicals use high dose antioxidants like melatonin (0.25-0.5mg/kg/night), curcumin (500mg), nigella sativa, dandelion, resveratrol (500mg) and liposomal glutathione.
To boost lagging neurotransmitter levels you can supplement the precursor amino acids: tyrosine and tryptophan (5-HTP) at 500-1000mg each per day, along with their cofactors: Zinc, Vitamins B6, B9, SAMe, and Magnesium.
In severe cases you can consider trying prescription intranasal steroids like dexamethasone 2mg daily, short acting insulin 20 IU daily, NMDA receptor antagonists like dextromethorphan (usually used as a cough syrup) or memantine (approved for use in Alzheimer’s).
A note on intranasal administration of meds: they have a direct access route to the brain and can prevent systemic side effects while delivering the medication right where it’s required. Intranasal insulin has healing effects and does not primarily act to lower blood glucose since neurons do not require insulin to take up glucose it has no effect on glucose utilization.
Intranasal meds can easily be administered by getting the liquid forms and drawing them up into a 1ml syringe to which is attached a cheap device called a nanoatomizer, when you depress the plunger on the syringe the liquid medication is released into the nose in a fine mist.

Supportive lifestyle interventions include intermittent fasting, ketogenic diet and dietary ketone esters.
Monthly repeat testing of the biomarkers will determine if the therapies are working.
Symptom improvement usually takes anywhere from 1-6 months at which point if labs are normalized I would consider trying to slowly taper. Most people can succesfully taper off meds and supplements within a year and get on with their lives.
If you’ve suffered from any symptoms of neuro-inflammation let me know below and also what you’ve done to treat it and how that has gone for you so far.







Great post! Exactly what I was looking for. I'm going to try getting some of the tests you listed from Sutter Healthcare to see if it can help solve my problem. I'm currently using telemedicine from Dr Kory. My LabCorp test results are an out-of-range high Spike antibody count: > 25,000 U/mL
LabCorp SARS-CoV-2 Spike Ab Dilution A, 01 >25,000 U/mL Negative<0.8
Roche Elecsys Anti-SARS-CoV-2 S
Thank you for your dedication to patients and truth-seeking! I am in your debt.
Lots of great information thanks. Should be very useful to many people right now.