Why Fat is Fit, or the Landfill Theory of Obesity
Toxicity and why your body doesn't make mistakes, even when it makes you fat
We used to live in Virginia Beach, which is on the coast obviously, and isn’t characterized by much topographical variety, i.e. it’s all flat, no hills to speak of, except there is one large anatopic (anachronistic, but of place not time) hill in the middle of a popular park. The mystery of the out of place hill is explained by the placards: this bulging beauty is actually a reclaimed waste dump, appropriately sealed I suppose and then soiled over, seeded, and voila, turned into a beautiful grassy knoll.
Keep this in mind as we discuss the link between toxins and obesity.
To begin with, I would wager that it’s actually better for many people to be fat than lean and no, I haven’t gone woke (or in other words insane), so just bear with me as I break it all down.
A little over a decade ago I was fresh out of residency and had gained a few dozen extra pounds. My wife and I stopped eating out, but ate whatever we wanted at home, including homemade organic spelt bread, complemented with lots of other whole foods like organic butter, eggs, milk, meat, fish, veggies, and fruit. The only thing we really made a point of avoiding altogether was added white sugar, though we replaced that with honey. Basically we made and ate whatever we wanted, including homemade desserts.
We were surprised when we lost weight effortlessly.
Then we gradually reverted back to our previous eating habits, i.e. eating out often and being less careful about ingredients and soon enough I was somewhat overweight again.
This time I decided to try a low carb, high fat, high protein diet that also eliminated various common trigger foods (the AIP or autoimmune paleo diet). This approach was at one point popularized as the Whole 30 diet, but recently they bent to Big Ag pressure and included seed oils in their eating plans, so they’re no longer fully AIP aligned, since seed oils are definitely not a paleo friendly food, requiring extensive modern industrial processing to make it possible to even stomach them, they are incredibly inflammatory, obesogenic and disease-causing.
So in this experiment I began eating lots of butter and low carb veggies with meat and fish on the side. I had been told it didn’t matter how much you ate on this plan, just eat your fill and you would naturally lose weight, because carbs are what actually make you fat, not fat or protein. Moreover, fat and protein were supposed to be the most satiating foods, so I wouldn’t have much appetite anyway. This eating plan was known far and wide as an easy way of dropping the pounds fast.
Strangely enough I didn’t lose weight, and I had a big appetite for what I was limiting myself to eating: veggies drenched in butter, meat and fish.
So eventually I dropped that and got distracted by life and stopped trying to lose the little bit of excess weight I had.
Then the pandemic hit, I came down with long COVID, and after a year of that my weight suddenly began to balloon alarmingly (some long haulers do lose weight, but that’s less common). Over the course of a year my weight shot up higher than I had ever seen before. I was 25% heavier than my previous body weight maximum. This was very uncomfortable and shocking to say the least.
At that point I went for a more holistic weight loss approach and documented it here:
I lost most of the weight I gained during the pandemic by focusing primarily on healthy sleep, circadian friendly light cycles, sunlight, walking, and generally healthy food.
But I plateaued well before I got back to where I had once been years before the pandemic. Also, as soon as I allowed some sweets my sugar cravings quickly reappeared and I soon gained back some of the weight I had just lost.
I thought I was essentially “allergic” to sugar, the way some people say they're allergic to alcohol, i.e. addicted to it, with no hope of moderating my intake. Unlike a lot of people I could get myself to go without sweets after enough self reflection and self motivation, but as soon as I started eating even a little bit of sugar again it would rapidly snowball into gorging on it.
At this point I began working closely with my friend Hakim Shabaz Ahmed.
We published a number of articles together and I followed along closely as he started helping many of my patients initiate deep healing from severe chronic diseases, while continuing to pro bono treat impoverished patients from around the world, where he had had his earliest successes with end stage cancer, autism, autoimmune disease, diabetes, obesity, heart disease, kidney disease, Alzheimer’s disease, etc. While even close friends and family had already benefited from his guidance, I had never felt I was sick enough to justify committing to his rather demanding protocols. I had kept looking for an easier way.
But, while I had been aware of his journey peripherally for many years, now I was more engaged with it and that involvement finally bred the motivation to finally take my own health seriously, because I deepened my appreciation for the importance of good health and the means of attaining it: detoxification of toxins and pathogens and replenishment of nutrients. These pillars of healing not only addressing the physical self, but all the higher levels as well including the intellect, emotions, thoughts, spirit, etc.
So I got a detailed detox program and supplement plan and dove into it as explained here:
I rapidly lost all the weight I had gained back, then shot past my recent low and got leaner than I had been in many years and after nearly 3 months the fat and inches were still dropping, though at a more reasonable rate. About 4 months in I stabilized, down a startling 27% from my peak weight. I still have just a bit of stubborn belly fat, but there’s good reason for that as we’ll discuss below (and I’m working on it).
On this detox and supplementation plan, which included a more modified version of a low carb paleo diet (only initially to help trigger detox), I found I had very little appetite at all, which certainly accounted for some of the rapid weight loss, but was strange in that I had been on a very similar diet in the past (as just described above) while retaining a significant appetite and not losing any weight.
The first two months with the greatest fat loss were easily explained because I was only eating low carb vegetables and fat, no high carb foods, grains and limited protein, no cooked meat, or fish and only 1 raw egg a day (for its nutrient density I did have 80 grams daily of liver and kidney). However after a couple months I added sardines and then a couple months after that added back in high quality meat and salmon, at which point I was basically back to the version of the AIP diet I had tried before that failed to moderate my appetite, except this time I didn’t experience the same unbridled appetite as I did then.
And then I went even further and added back select grains: mostly amaranth and buckwheat, abandoning the very low carb aspect of the diet entirely. This initially increased my appetite minimally since I had been avoiding grains for so long, though subsequently in the following couple months appetite trended back to baseline. Despite these additions there was no increase in my weight and my appetite was still far lower than it had been on that first AIP attempt where I lost no weight.
It soon became clearer to me how applicable were the ongoing refrains that have characterized this blog over the last few months:
all diseases are due to two primary causal categories: a. excess of harmful things, i.e. primarily toxicity/pathogenicity and b. lack of beneficial/essential things, e.g. nutrient, or ore broadly speaking nourishment deficiencies.
the body does not typically make mistakes broadly speaking, so disease manifestations are usually in some way helping to fix and/or signal that there is some deeper problem that needs to be addressed, i.e. symptoms are but a message and/or maneuver.
So being overweight comes primarily from toxicity and nutrient deficiency, like all diseases.
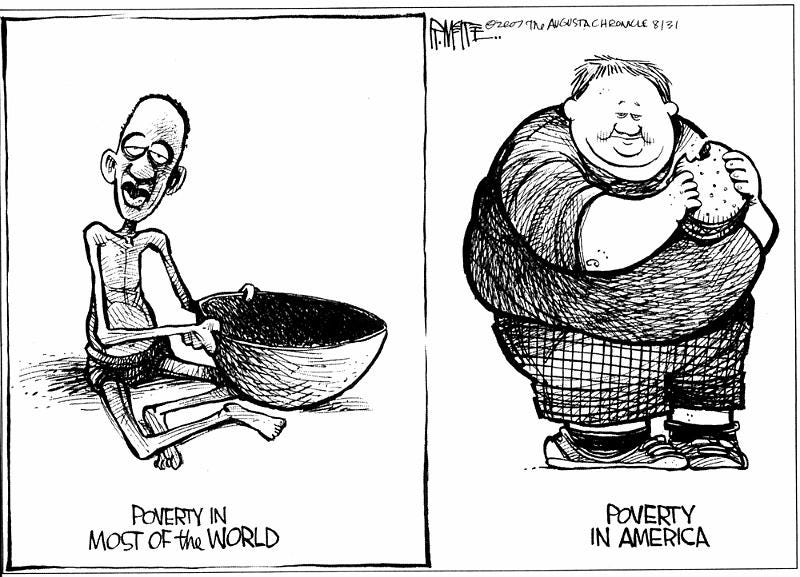
As explained earlier in the below post, the best way to conceive of excess weight overall is as starvation: lack of necessary nourishment. The toxicity side of the equation in this paradigm can be conceived as an additional burden weighing upon nutrient sufficiency and organ functioning, when energy systems collapse and can no longer keep up with toxin destruction and expulsion, there is nothing left to do but store them within.
Ozempic: Sabatoge by Siege Because Obesity is Really Starvation
Toxicity may begin, as most toxicity does, at the level of the emotional being. Perhaps someone eats their feelings, or feels unsafe and needs a buffer from other people.
The important point to understand is that emotional imbalance doesn’t just remain at the level of the emotional self, it leads inevitably to physical organ imbalances, e.g. of the thyroid, pancreas, adrenals, kidneys, liver, fat tissue, and more. These organs and tissue variously affect metabolism, insulin sensitivity, stress hormone levels, detoxification, etc - all functions that impact body weight. When these organs come under stress they burn through more nutrients than normal until they become deficient in micronutrients. This weakens them and makes them prone to toxin accumulation.
We’re awash in a sea of toxins from before birth, being exposed even in the womb, so if our natural detox systems begin to fall behind, many of those toxins bioaccumulate, or start to fill up our tissues, rather than being expelled from the body, and this leads to toxicity. As tissues become dragged down by ongoing toxicity, pathogens make inroads, in some cases helping to sequester toxins, in others simply multiplying because our host defenses are down. The immune system does its best to root out the toxins and fight off the pathogens, and this means there is inflammation, which means there are various symptoms.
Getting back to weight gain: many toxins are lipophilic, meaning fat-loving, i.e. they are attracted to and bind with fat, so fat in effect acts as a storage depot for toxins, which may sequester them away from where they can actively cause damage in our other tissues.
Could it be that our bodies, sensing a losing battle with toxicity, actually decide to mitigate the damage by locking up many toxins and pathogens in fat depots, the bodies own version of a landfill hiding beneath a public park on the one hand, and mass incarceration of criminals on the other?
FAT LOVING TOXINS
These are many common pervasive modern environmental toxins for which studies have confirmed storage in human adipose tissue:
Persistent Organic Pollutants (POPs)
Polychlorinated Biphenyls (PCBs): Used in electrical equipment, now banned but persists in the environment.
Dioxins: Byproducts of industrial processes, including waste incineration.
Organochlorine Pesticides:
DDT and its metabolites (DDE): Widely studied for accumulation in fat tissue.
Lindane: An insecticide used in agriculture and pharmaceuticals.
Hexachlorobenzene (HCB): A fungicide and industrial byproduct.
Brominated Flame Retardants
Polybrominated Diphenyl Ethers (PBDEs): Found in furniture, electronics, and textiles.
Heavy Metals (Indirect Storage via Fat Binding)
Methylmercury: While primarily stored in the brain and organs, it can bind to fatty tissues indirectly.
Lead and Cadmium: Known to affect fat indirectly, though stored primarily in bones and organs.
Lipophilic Pharmaceuticals
These can accumulate in fat, especially over prolonged exposure (see next section).
Plasticizers
Phthalates: Found in plastics, confirmed to bioaccumulate in adipose tissue.
Industrial Chemicals
Perfluoroalkyl and Polyfluoroalkyl Substances (PFAS): Used in non-stick cookware and water-repellent fabrics.
PERSISTENT (P)HARMA TOXINS
Lipophilic (fat-soluble) pharmaceuticals have a high affinity for adipose (fat) tissue, leading to their potential accumulation and prolonged action in the body. Below is a categorized list of commonly known lipophilic pharmaceuticals, organized by therapeutic class:
Anesthetics: Propofol, Thiopental, Ketamine, Halothane, Isoflurane, Sevoflurane.
Sedatives & Hypnotics:
Benzodiazepines: Diazepam, Lorazepam, Clonazepam, Alprazolam.
Z-Drugs: Zolpidem, Eszopiclone.
Antidepressants & Antipsychotics:
SSRIs: Fluoxetine, Sertraline, Paroxetine.
TCAs: Amitriptyline, Imipramine, Nortriptyline.
Antipsychotics: Clozapine, Olanzapine, Quetiapine, Risperidone.
Opioids: Fentanyl, Methadone, Buprenorphine, Oxycodone.
Anticonvulsants: Phenytoin, Valproic Acid, Phenobarbital.
Hormones & Steroids: Prednisone, Dexamethasone, Estrogen, Testosterone, Progesterone.
Antimicrobials:
Antibiotics: Rifampin, Erythromycin, Linezolid.
Antifungals: Ketoconazole, Itraconazole, Fluconazole.
Anticancer: Tamoxifen, Doxorubicin, Paclitaxel, Docetaxel.
Lipid-Lowering Drugs: Atorvastatin, Simvastatin.
Miscellaneous: THC, CBD, Propranolol, Metoprolol, Cyclosporine, Tacrolimus, Chloroquine, Mefloquine.
TOXINS & OBESITY
There is evidence suggesting that an excess toxic load in the body can contribute to obesity, and this may serve as a protective mechanism to sequester toxins in fat tissue and reduce their harmful effects on other vital tissues. This concept is supported by research linking environmental toxins, persistent organic pollutants (POPs), and certain pharmaceuticals to disrupted metabolic processes and obesogenic effects.
Evidence for Toxins Contributing to Obesity
1. Disruption of Metabolic Pathways
Many toxins, such as PCBs, dioxins, and phthalates, act as endocrine disruptors, interfering with hormones that regulate metabolism, appetite, and fat storage.
Leptin and Insulin Resistance: Toxins can impair leptin and insulin signaling, leading to increased hunger and fat storage.
Thyroid Function: POPs and heavy metals disrupt thyroid hormone balance, slowing metabolism and promoting weight gain.
2. Obesogens
Certain chemicals, known as obesogens, actively promote the formation and growth of adipose tissue. Examples include:
Bisphenol A (BPA)
Phthalates
Perfluoroalkyl substances (PFAS)
These chemicals:
Increase fat cell differentiation: Stimulate pre-adipocytes to become mature fat cells.
Promote fat accumulation: Enhance lipid uptake and storage in adipocytes.
3. Protective Sequestration in Fat Tissue
Fat tissue acts as a storage depot for lipophilic toxins, effectively isolating them from circulation to protect vital organs like the brain, liver, and kidneys.
This protective mechanism reduces acute toxicity but may lead to chronic, low-grade inflammation in fat tissue.
As toxic load increases, the body may expand fat stores to accommodate the additional toxins, contributing to obesity.
4. Chronic Inflammation and Weight Gain
Many toxins stored in fat tissue trigger inflammatory pathways, including the release of cytokines and adipokines, which:
Promote further fat deposition.
Create a feedback loop of inflammation and metabolic dysfunction.
5. Evidence from Weight Loss Studies
During rapid weight loss, stored toxins are released back into circulation as fat is broken down, leading to:
Increased oxidative stress and inflammation.
Temporary metabolic dysregulation, potentially making sustained weight loss more challenging.
Studies have shown that individuals with higher toxin levels may experience:
Slower fat loss during weight reduction programs.
Greater difficulty maintaining weight loss.
Protective Role of Fat Storage
The sequestration hypothesis suggests that adipose tissue expansion in response to toxic load:
Spreads the burden: Limits the concentration of circulating toxins to reduce harm to vital organs.
Buffers metabolic disruptions: Prevents acute systemic effects of lipophilic toxins.
Delays toxicity onset: Provides a "safe" storage site, at least temporarily, for otherwise harmful compounds.
So, excess toxic load in the body appears to have an obesogenic effect, driven by:
Endocrine disruption.
Inflammation.
Protective sequestration of toxins in fat tissue.
While this process protects vital organs, it can also lead to chronic metabolic dysfunction and increased fat storage. Addressing the root causes of toxin exposure, improving detoxification pathways (e.g., liver and kidney function), and supporting a healthy metabolism are key strategies to mitigate these effects.
The Toxin That Must not be Named: Non Native EMF
One cellular toxin deserves its own treatment. It is not usually thought of as a toxin, and not usually considered to affect human health at all, despite decades of research to the contrary and 10s of thousands of published papers.
The reason it flies under the radar is that it’s a necessary component of military communications and readiness, and as such the State has endeavored to essentially cover it up, using the same tactics that were used to attempt a cover up of the COVID vaccine side effects. However in the case of this far more pervasive toxin they were largely successful, at least until now (RFK Jr is aware of the problem, so hopefully as HHS Secretary will bring the research to light, conduct further studies and eventually create healthy exposure guidelines that lead to human friendly versions of these necessary technologies).
Electromagnetic fields (EMFs) have been suggested to influence metabolism, obesity, and overall energy regulation through various mechanisms. While research is still evolving, here are some potential ways EMFs may contribute to overweight and obesity:
1. Disruption of Melatonin and Circadian Rhythms
EMFs, particularly artificial blue light and radiofrequency (RF) radiation, can suppress melatonin production and disrupt circadian rhythms. Melatonin plays a role in metabolism and fat regulation, and lower levels are linked to increased fat storage and insulin resistance.
Disrupted sleep from EMF exposure can also alter hunger hormones (ghrelin, leptin), leading to increased appetite and weight gain.
2. Impact on Mitochondrial Function and Energy Production
EMFs cause oxidative stress and impair mitochondrial function, leading to reduced ATP production and metabolic inefficiency. Poor mitochondrial function can contribute to fat accumulation and difficulty in burning calories efficiently.
3. Influence on Calcium Signaling and POMC Pathway
EMFs increase intracellular calcium (via voltage-gated calcium channels, VGCCs), leading to dysregulation of the POMC (pro-opiomelanocortin) pathway. The POMC pathway in the hypothalamus is crucial for regulating energy balance and metabolism. EMF-induced calcium overload may disrupt this pathway, leading to increased insulin resistance and fat storage.
4. Increased Insulin Resistance and Blood Sugar Dysregulation
Studies suggest radiofrequency EMFs (from WiFi, cell phones, etc.) may impair glucose metabolism, leading to higher fasting insulin and a greater tendency for fat storage. Increased insulin resistance means the body is less efficient at using glucose for energy, promoting weight gain and obesity.
5. Disrupting Hormonal Balance
EMFs can affect thyroid function, reducing T3/T4 hormone levels, which are critical for metabolism. Some studies suggest EMF exposure may increase cortisol (stress hormone), which promotes fat accumulation, especially visceral fat.
6. Altered Gut Microbiome
Emerging research suggests EMFs may disrupt the gut microbiome, leading to dysbiosis, which is linked to obesity, inflammation, and metabolic syndrome. A disrupted gut microbiome can also impair nutrient absorption and energy balance, promoting weight gain.
7. Decreased Brown Fat Activation
Brown adipose tissue (BAT) is important for thermogenesis (heat production) and fat burning. Some researchers speculate that chronic EMF exposure reduces BAT activation, decreasing the body’s ability to burn excess fat.
To sum up, while definitive human studies are still lacking, there is strong mechanistic evidence suggesting that chronic EMF exposure may contribute to weight gain, metabolic dysfunction, and obesity. The combination of disrupted circadian rhythms, increased insulin resistance, mitochondrial dysfunction, hormonal imbalance, and gut microbiome changes could make it harder to regulate weight.
If concerned about EMFs and their metabolic effects, strategies such as reducing exposure to artificial blue light, minimizing RF exposure (e.g., WiFi, cell phones), improving sleep quality, and optimizing mitochondrial function may help mitigate their potential impact.
One radical move I’ve been contemplating is to sleep within a Faraday cage, which effectively blocks EMF signals. A simple Faraday cage can be constructed from a fine silver or copper mesh, which can be woven into a fabric and hung around the bed like mosquito netting and will block almost all nnEMF penetration and could be particularly helpful when severe chronic disease has made a mess of a patients bioelectrical systems.
MICRONUTRIENT DEFICIENCY & OBESITY
What about the nourishment side of the chronic disease equation? Doesn’t obesity mean there is over nourishment, rather than mal or under nourishment?
Not quite.
Micronutrient deficiencies are increasingly recognized as a causative mechanism of obesity, influencing the development and persistence of excess weight. This relationship is rooted in how deficiencies in essential vitamins and minerals disrupt metabolic, hormonal, and behavioral processes, leading to overeating, impaired energy balance, and fat storage, as well as how deficiencies lead to the exhaustion of detoxification systems, as explained earlier.
As I’ve written about before, obesity is really a type of starvation (though not just of chemical micronutrients, but sunlight, darkness, sleep, movement, physical and emotional intimacy, connection, meaning, purpose, etc - all of these snowballing to drive people towards consuming more of whatever is available, even if it’s not fulfilling the real deficiencies).
Mechanisms Linking Micronutrient Deficiency to Obesity
1. Disrupted Appetite Regulation
Deficiencies in specific micronutrients can impair the body's ability to regulate hunger and satiety, leading to overeating:
Magnesium, Zinc, and Chromium:
These are involved in insulin signaling and glucose regulation.
Deficiencies can lead to insulin resistance and sugar cravings.
Vitamin D:
Low vitamin D levels impair leptin signaling, a hormone that tells the brain you're full.
This contributes to overeating and increased fat storage.
2. Metabolic Slowdown
Micronutrients are cofactors for enzymes involved in energy production and fat metabolism:
Iodine, Selenium, and Iron:
Essential for thyroid hormone production, which regulates metabolic rate.
Deficiencies slow metabolism, leading to reduced energy expenditure and fat accumulation.
B Vitamins:
Key players in carbohydrate, protein, and fat metabolism.
Deficiencies lead to fatigue and reduced physical activity, contributing to a positive energy balance.
3. Impaired Fat Burning (Lipolysis)
Carnitine (a micronutrient synthesized from lysine and methionine):
Deficiency reduces the transport of fatty acids into mitochondria for energy production, resulting in fat accumulation.
Zinc:
Deficiency impairs lipid metabolism by reducing enzyme activity involved in fat breakdown.
4. Increased Fat Storage via Inflammation
Micronutrient deficiencies contribute to chronic low-grade inflammation, which promotes fat storage:
Omega-3 Fatty Acids:
Deficiency leads to a pro-inflammatory state, increasing adipose tissue growth.
Magnesium:
Low levels exacerbate inflammation and insulin resistance, driving obesity.
5. Altered Gut Microbiome
Micronutrients like zinc, vitamin D, and magnesium are critical for a healthy gut microbiome.
Deficiencies disrupt the gut microbial balance, increasing energy extraction from food and promoting fat storage.
6. Food Cravings and "Hidden Hunger"
When the body lacks essential nutrients, it can trigger cravings for high-calorie, nutrient-poor foods in an effort to compensate:
Calcium Deficiency:
Associated with cravings for dairy or high-fat foods.
Iron Deficiency:
Linked to cravings for meat or sugary foods.
7. Oxidative Stress and Adipocyte Dysfunction
Antioxidants like vitamins A, C, and E, as well as selenium, protect cells from oxidative damage:
Deficiency increases oxidative stress in adipocytes, leading to dysfunction and abnormal fat storage.
8. Exhaustion of Detox Pathways and Toxin Storage
Micronutrient deficiencies can impair the liver and other detoxification organs by reducing the efficiency of key enzymes involved in toxin metabolism and elimination:
Inadequate levels of antioxidants (such as vitamins A, C, E, and selenium) and certain B vitamins compromise detoxification processes, leading to the buildup of toxins. These accumulated toxins are often sequestered in fat tissues—a protective mechanism that, over time, contributes to further fat accumulation and obesity.
Selected Supporting Evidence
Vitamin D and Obesity:
Studies show obese individuals are often vitamin D deficient, potentially due to sequestration in fat tissue.
Supplementation has been linked to improved weight loss outcomes in vitamin D-deficient individuals.
Magnesium and Insulin Sensitivity:
Magnesium deficiency is highly prevalent in people with obesity and correlates with insulin resistance and higher body weight.
Zinc and Appetite Control:
Zinc supplementation in deficient individuals has been shown to reduce appetite and improve weight management.
B Vitamins and Energy Metabolism:
B12 and folate deficiencies are more common in obese individuals, impairing energy metabolism and physical activity.
So, micronutrient deficiencies definitely disrupt metabolic and hormonal pathways, contributing to the development and persistence of obesity. Addressing these deficiencies through dietary changes or supplementation can:
Improve appetite regulation.
Enhance energy expenditure.
Reduce inflammation.
Support overall metabolic health.
This all strongly suggests that addressing "hidden hunger" (micronutrient deficiencies) is a crucial strategy for tackling obesity and its associated health risks.
PUTTING IT ALL TOGETHER
There are many ways to lose weight fast or slow. Some require a lot of willpower to sustain and others do not. Any system can be hacked to achieve an outcome at odds with the system inputs, but the hackers mindset belies a deep misunderstanding of the actual meaning of the illness state, in this case being overweight.
It’s not the fatness that is the problem, it’s the toxins that the body is trying to neutralize by weight gain that are usually the real problem on the one hand, with nutrient deficiencies contributing to a “starvation” state on the other.
Forcing weight loss by some metabolic, or micronutrient maxing, or caloric restriction, or exercising, or medication hack will not necessarily solve the toxicity. In fact it could worsen it by releasing toxins into systemic circulation without having previously opened detox pathways for elimination, so as they circulate, tapped within, they will just damage all tissues.
If the body makes a decision to increase fat stores, it does so for good reason. It is the best of all possible outcomes, given the situation you’ve put yourself in.
DETOXIFICATION FOR WEIGHT LOSS
So how do you detoxify properly in order to lose weight effortlessly by sending the body the signal that it no longer needs to stimulate weight gain to sequester toxins?
Slow and steady wins the race.
Your body is a crowded theater that’s on fire. If everyone runs for the exits all at once no one will make it out. The way will be blocked.
It’s the same with throwing out the toxins that are slow-burning your body down.
Detoxification requires relaxation, in other words good autonomic nervous system activity, rather than sympathetic excess. The autonomic nervous system is the “rest and digest and detox” arm of the nervous system. It’s the nighttime, letting-go, out-breath yin to the daytime taking-in-breath yang.
Detoxification requires supporting the organs that detoxify and excrete: the immune system, skin, lungs, liver/gallbladder, kidneys/bladder, and vascular systems (especially draining veins and lymphatics).
It requires proactively stimulating those processes that expel toxins, like sweating, deep breathing, hydrating/urinating, eating/defecating, etc.
We can assist our body’s natural detoxification pathways by binding toxins that are on their way out but may be reabsorbed before final exit by using tools like chlorella, which gently sucks toxins out of circulation without greatly impacting nutrients as some other binders do.
Herbs like moringa and food like broccoli sproutscan help us neutralize xenoestrogens.
Along the way we can start to cull the various microorganisms that have overgrown in response to the toxins, like mold which binds heavy metals and helps shield from nnEMFs, using broad spectrum antimicrobials like chlorine dioxide, and various antimicrobial herbs.
There is a lot and the specific plan, including the elements and their sequence, depends heavily on the specifics of each person’s situation. I wish there was something simple and straightforward enough that would work for everyone, but in such a world we wouldn’t be surrounded by the beauty of the varied and complicated expressions of humanity that help make life interesting and worthwhile.
The only way to heal from anything, including obesity and overweight, is individually, 1 on 1 with a master healer. Even masters struggle to heal themselves given the difficulty of maintaining proper perspective and resisting the urge to go too easy, or too hard.
If you’re ready to take the journey to deep healing, get in touch with us at mygotodoc.com/hakim.